Medicaid pharmacy carve out the right solution for Kentucky taxpayers
Published 1:46 pm Friday, January 10, 2020
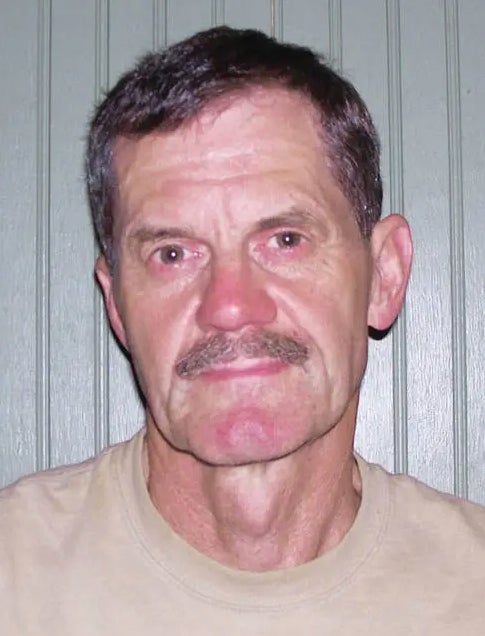
By Don Kupper
President of the Kentucky Pharmacists Association
For many Kentuckians, a trip to the pharmacy is a routine part of maintaining good health. But behind the scenes, the process of getting your prescription is proving to be much more complex—and costly—than necessary. And as a taxpayer, you’re likely paying for it whether you go to the pharmacy or not.
A significant portion of the prescriptions written in Kentucky are for the 1.3 million individuals enrolled in the state’s Medicaid managed care program. Last year, nearly $1.7 billion went toward prescription medications for Medicaid managed care beneficiaries. These numbers reflect Medicaid’s role as a critical lifeline for many of our communities’ most vulnerable. We must remain mindful, though, that the program’s size and scope are made possible by taxpayer dollars—and we should be doing everything possible to ensure the state is being a good steward of those funds.
This has been an ongoing conversation among state leaders, and with a new legislative session around the corner, more discussions will be taking place on how we can better contain costs while protecting access to health care within the Medicaid program. One important step already in motion is beginning to pull back the veil on the powerful, shadowy middlemen that have a heavy hand in determining what Kentuckians pay out-of-pocket for their prescription medications: pharmacy benefit managers, or PBMs.
Despite the outsized role PBMs play in determining prescription drug costs, most consumers know very little, if anything, about what they do and how Kentuckians’ hard-earned tax dollars are contributing to PBMs’ rapidly increasing profit margins.
Under the current setup, Medicaid managed care organizations (MCOs) contract with PBMs to deliver pharmacy benefits to enrollees. This has led to increased costs for Kentucky taxpayers and more administrative hoops for pharmacists to jump through to get their patients the treatments they need. In some cases, PBMs have gone so far as to cut community pharmacists out of the equation entirely, directing patients to utilize impersonal mail-order pharmacies.
For far too long, PBMs have been allowed to operate with virtually zero oversight and to profit at the expense of Kentucky patients, providers and taxpayers. A slew of legislative hearings, state-commissioned reports and news articles have shown how they use a sneaky practice called “spread pricing” to generate profits at taxpayers’ expense. Last year alone, PBMs raked in $123 million in profits by charging the state far more than the actual cost of the medication being dispensed—and this practice continues today.
This is why legislation will be introduced in 2020 to eliminate PBMs’ undue influence by “carving out” the pharmacy benefit from Kentucky’s Medicaid program in favor of a much simpler and more transparent fee-for-service model that will benefit patients, providers and taxpayers.
When we drop the middleman, we’re able to create a more streamlined health care system, ensuring fewer barriers to care for patients and giving back valuable time and resources to pharmacists and other care providers. In fact, a recent initial report from the Department of Medicaid Services, which is still under review, shows that carving out the pharmacy benefit could save Kentucky many millions of dollars each year.
While the carve out serves all Kentuckians well, it is particularly critical for the Commonwealth’s community pharmacists, who have been shuttering their doors in rising numbers as their costs to stay afloat continue to rise. These closures are especially problematic in rural areas, where such an event could extend a resident’s trip to the pharmacy by not just minutes but hours.
There is no doubt that Medicaid serves a crucial role in our state, and if we truly want to improve health outcomes for its beneficiaries, our elected leaders in Frankfort must ensure we’re spending budget dollars wisely. In the new year, it can start with streamlining pharmacy benefits and putting patients and providers—rather than profit-driven PBMs—first.
Don Kupper is a third-generation pharmacist who has been practicing for 38 years in a variety of settings. He now works as a local consultant and compliance manager for a compounding pharmacy while also serving as President of the Kentucky Pharmacists Association.